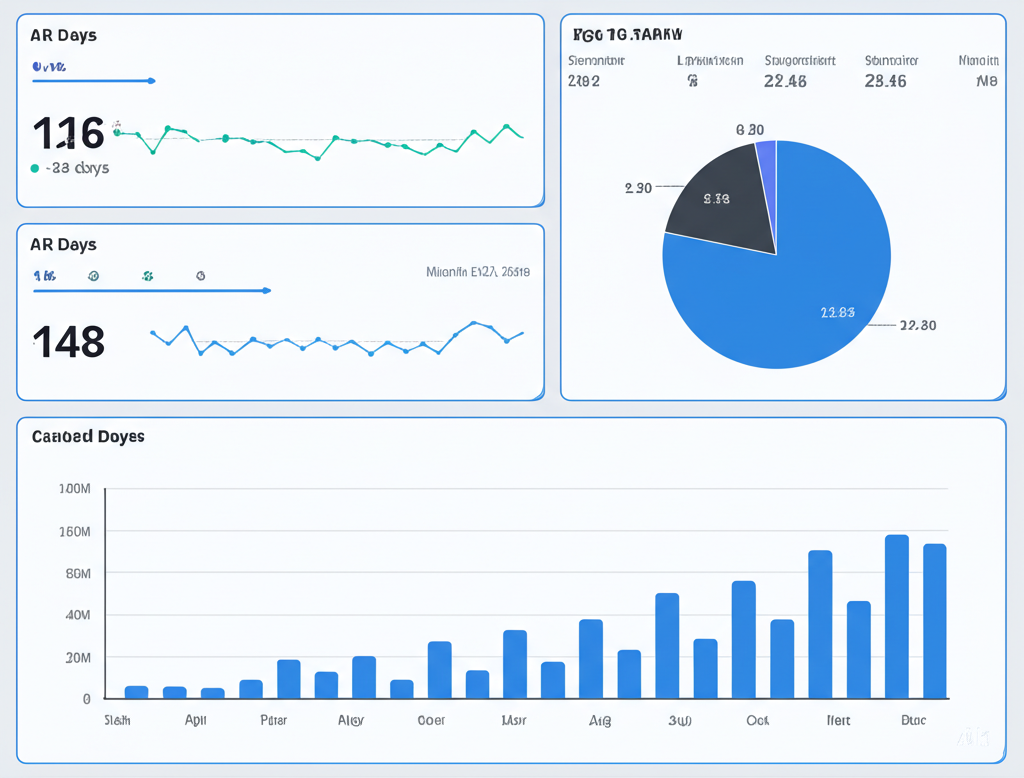
35% fewer A/R days
Multi-specialty clinic reduced A/R days and improved cash flow with eligibility and coding automation.
Learn moreCollect Easy AI turns patient records into billable claims, verifies eligibility, and streamlines patient collections. Ethical by design, with self‑service that improves outcomes and satisfaction.
Automation where it matters, transparent control where you need it.
Securely connect popular EHRs and import encounters, notes, and benefits data.
We parse notes and ICD/CPT mappings to draft billable claims for review.
Eligibility checks and edits before clean claim submission to payers.
Friendly patient portal for statements, AutoPay, and payment plans.
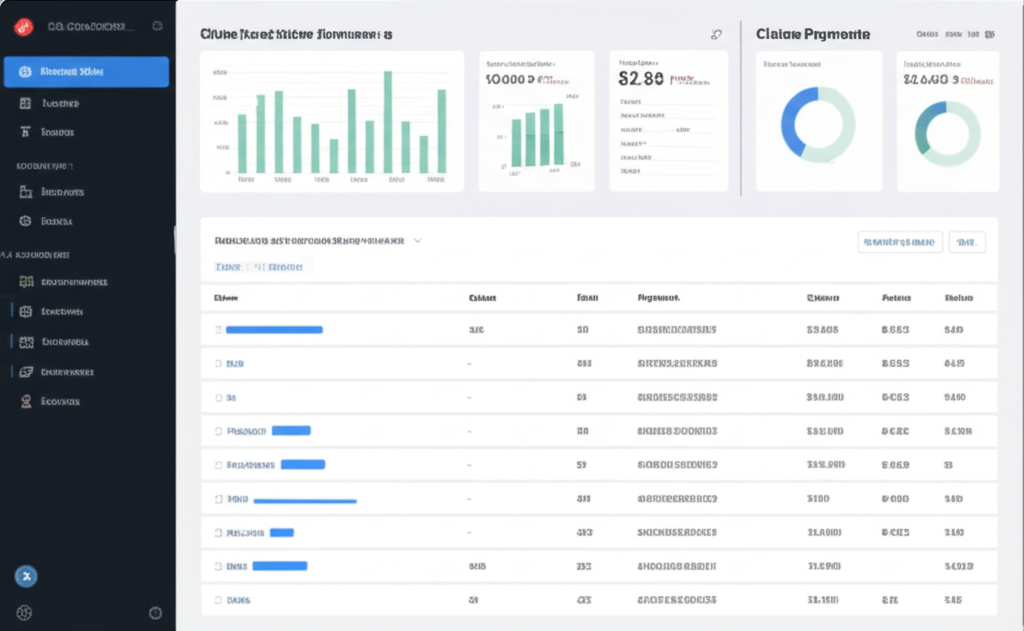
Realtime A/R, denial trends, and collection performance dashboards.
Draft ICD/CPT/HCPCS with audit trails and human-in-the-loop review.
Auto-check coverage and benefits to reduce denials upfront.
Surface root causes and recommended edits to speed resubmissions.
Self-service statements, AutoPay, plans, and digital wallets.
A/R days, collection rate, write-offs, and payer performance.
Encryption in transit/at rest, role-based access, SSO.
Automation that respects patients and accelerates cash.
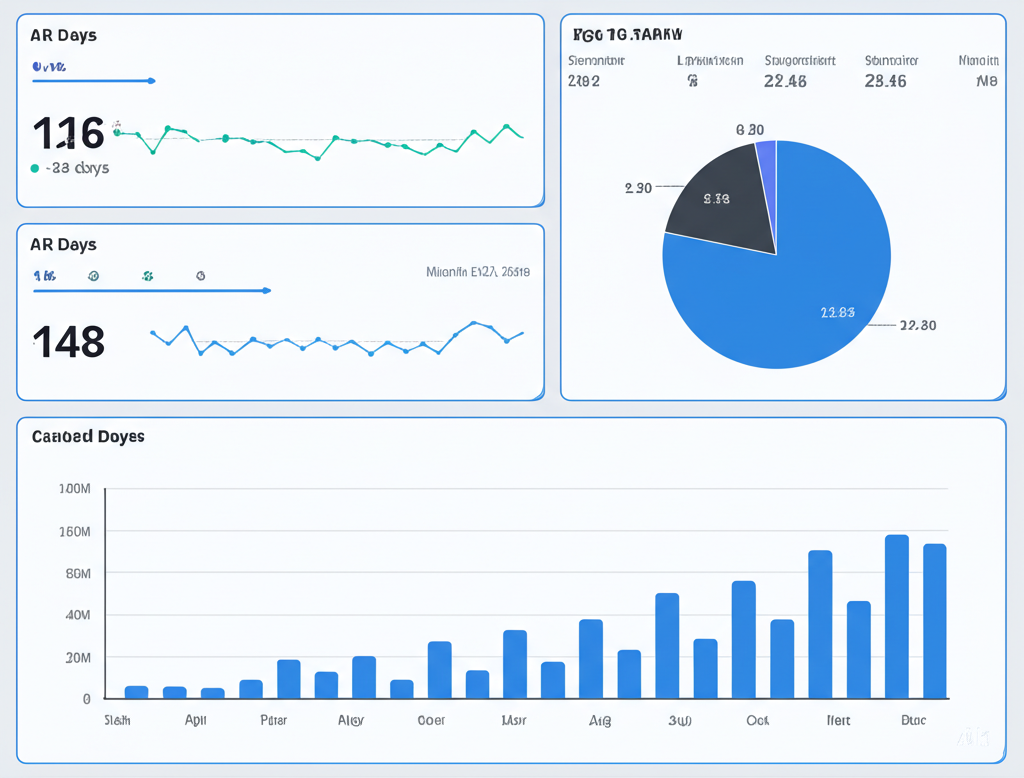
Multi-specialty clinic reduced A/R days and improved cash flow with eligibility and coding automation.
Learn more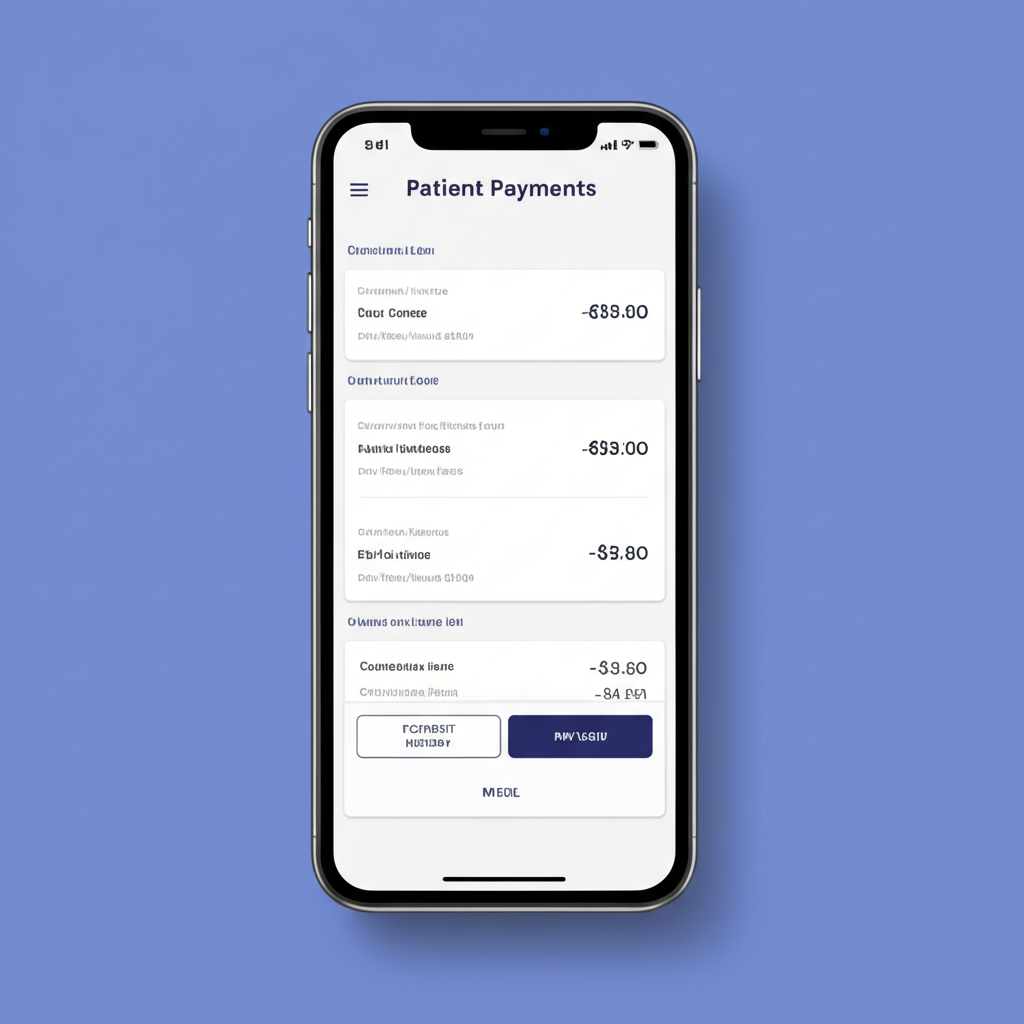
Self-service portal and AutoPay increased patient collections without added staff.
Learn more
Proactive edits and benefits checks cut top denial codes for a cardiology group.
Learn more
Claims prepared in minutes with AI-assisted coding and reviewer workflows.
Learn more
Transparent statements and payment plans improved satisfaction scores.
Learn more
Progress rooted in compliance and outcomes.
On a mission to make billing ethical, accurate, and effortless.
We started with a simple idea: use AI to reduce administrative burden while improving patient clarity and outcomes.
Early access for multi-specialty groups and RCM partners.
Our human-in-the-loop workflows paired with draft codes and audit trails to accelerate clean claims.
Transparent statements, AutoPay, and payment plans.
Practices saw higher collections and better patient satisfaction from clear digital statements and options.
Proactive coverage checks and denial trend surfacing.
Teams reduced top denial codes with recommended edits before submission, cutting avoidable rework.
See how AI can accelerate accurate billing and patient‑friendly collections.
Insights on AI-assisted coding, eligibility, and patient payments—no spam.